Okay, let’s talk about this Health Alliance thing and weight loss meds. I actually went through trying to figure this out myself not too long ago.
My Little Investigation
So, I started wondering about weight loss medications, you know, the ones people talk about sometimes. The big question for me was, does my insurance, Health Alliance, actually help pay for them? Because let’s be real, that stuff can be pricey.
First thing I did was grab my laptop. I figured the best place to start was their website. Trying to call customer service sometimes feels like a whole afternoon project, and I wanted answers faster.
I logged into my member account on the Health Alliance site. Had to reset my password, naturally, because who remembers all these things? Once I got in, I started poking around. Looked for sections like ‘My Benefits’ or ‘Coverage Details’.
It wasn’t immediately obvious where to find info on specific types of drugs. I found something called a ‘Formulary’ which I guessed was just their list of covered drugs. Seemed like the right place.
Digging into the Drug List
This formulary thing was a big document, like a PDF file. I had to use the search function (Ctrl+F is your friend!). I typed in ‘weight loss’ and also the names of a couple of specific medications I had heard about.
- Searched for general terms first.
- Then tried specific drug names.
- Looked for notes or codes next to the drug names.
What I found was… well, it wasn’t a simple yes or no for everything. For my specific plan, it looked like some medications might be covered, but often needed something called ‘prior authorization’. That means the doctor has to send paperwork to Health Alliance explaining why you need it before they’ll agree to cover it. Sometimes there were specific rules, like you had to have a certain BMI or other health conditions.
What I Learned
So, does Health Alliance cover weight loss medication? For me, the answer was “maybe, with conditions.” It really depended on the specific drug and meeting their requirements.
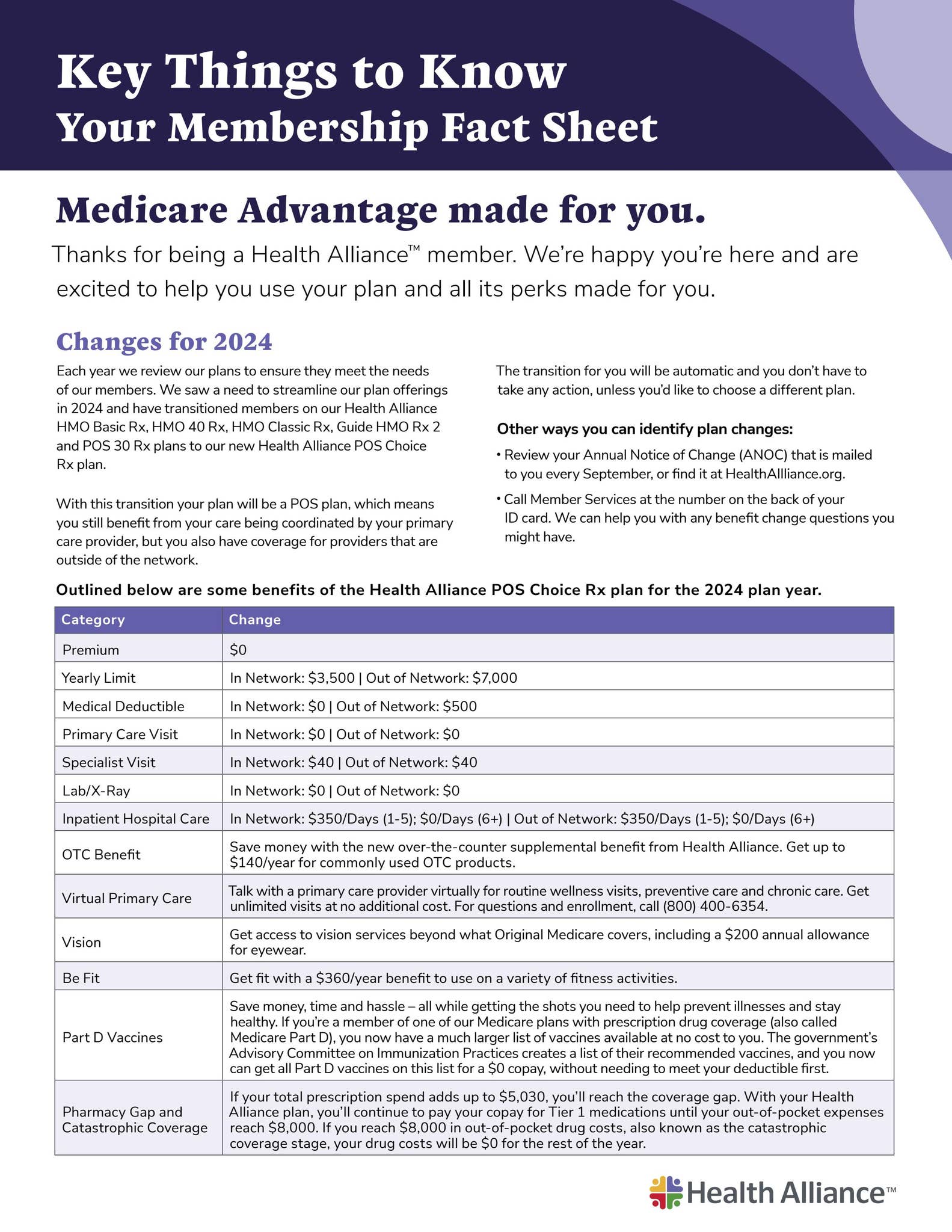
The most important thing I figured out is that you really have to check your own specific plan details. Don’t just take someone else’s word for it because plans can be different. Logging into your member portal and checking that formulary or list of covered drugs is the way to go. If it’s confusing, then maybe make that call to customer service, armed with what you found online. That was my process, anyway. Hope sharing this helps someone else navigate it!